AdemolaOkubena
Rookie
- Nov 20, 2013
- 7
- 3
- 0
- Banned
- #1
hello friends,
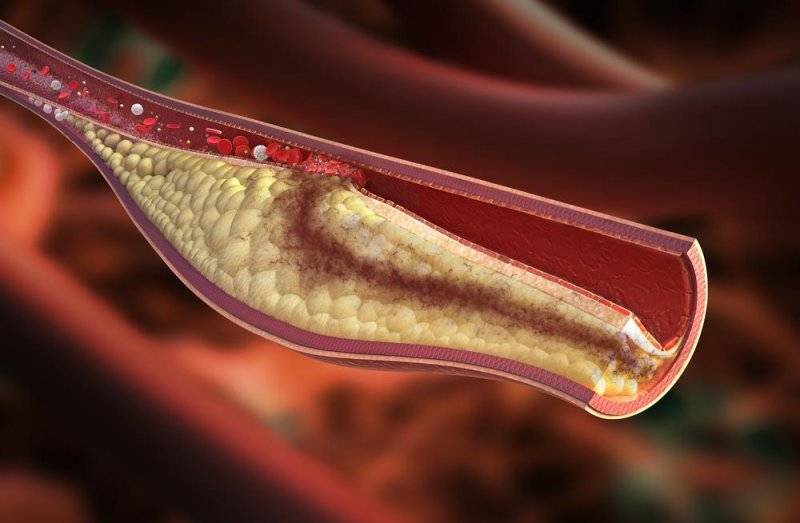
My friend is always going to gym for body building. He don't know, he is a blood pressure patient. There is no side effect but he takes medicine as per doctors pescribed. The doctor gives some instruction which food you have taken for blood pressure. Cholesterol disease have seen amon the people. A person who is eating fast food they suffer cholesterol disease. It is bad for health. Now the doctors strictly suggested don't eat fast food.
Thanks a lot
Ademola Okubena
My friend is always going to gym for body building. He don't know, he is a blood pressure patient. There is no side effect but he takes medicine as per doctors pescribed. The doctor gives some instruction which food you have taken for blood pressure. Cholesterol disease have seen amon the people. A person who is eating fast food they suffer cholesterol disease. It is bad for health. Now the doctors strictly suggested don't eat fast food.
Thanks a lot
Ademola Okubena