Menerva Lindsen
Active Member
- Dec 18, 2014
- 231
- 23
- 33
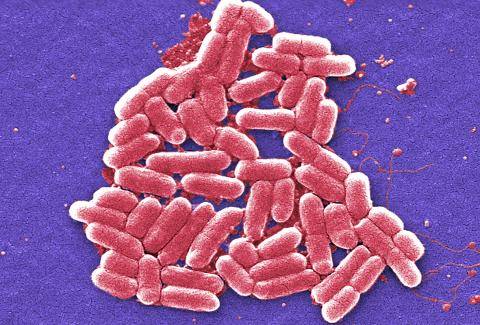
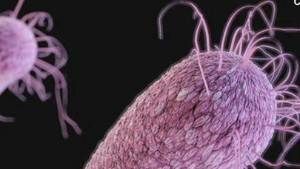
The term "nightmare bacteria" does not bode well for anyone who may get infected.
That's what CDC epidemiologists call carbapenem-resistant Enterobacteriaceae, or CRE, which kill up to half the patients who contract them.
The family of superbugs made headlines two years ago when the Centers for Disease Control and Prevention warned it was spreading.
Now, they're back in the news after seven patients at a Los Angeles hospital caught CRE after routine endoscopic treatments for bile ducts, gall bladder or pancreas.
Two of them have died, the Ronald Reagan UCLA Medical Center said Wednesday. CRE was a contributing factor in the deaths, but the exact cause of the deaths wasn't immediately disclosed, a hospital spokeswoman said. The medical center is contacting 179 others who had endoscopic procedures between October and January. It's offering them home tests to screen for the bacteria.
Understanding CRE the nightmare superbug that contributed to 2 deaths in L.A. - CNN.com
What kind of divine punishment will we face in future? How easy may we die in the USA? We are dieing because of guns, drugs, bad food and ecology. Moreover new bacterias are appearing to destroy our nation!!!
That's what CDC epidemiologists call carbapenem-resistant Enterobacteriaceae, or CRE, which kill up to half the patients who contract them.
The family of superbugs made headlines two years ago when the Centers for Disease Control and Prevention warned it was spreading.
Now, they're back in the news after seven patients at a Los Angeles hospital caught CRE after routine endoscopic treatments for bile ducts, gall bladder or pancreas.
Two of them have died, the Ronald Reagan UCLA Medical Center said Wednesday. CRE was a contributing factor in the deaths, but the exact cause of the deaths wasn't immediately disclosed, a hospital spokeswoman said. The medical center is contacting 179 others who had endoscopic procedures between October and January. It's offering them home tests to screen for the bacteria.
Understanding CRE the nightmare superbug that contributed to 2 deaths in L.A. - CNN.com
What kind of divine punishment will we face in future? How easy may we die in the USA? We are dieing because of guns, drugs, bad food and ecology. Moreover new bacterias are appearing to destroy our nation!!!