abu afak
ALLAH SNACKBAR!
- Mar 3, 2006
- 7,677
- 2,694
- 315
What do they do with these people? Do they stay infectious (by blood/mosquito/etc) even if they recover?
Cases have been found internationally, now here.
Many (if not all) bacterial bugs, it seems, can get resistance on the genetic level.
(see Carbapenem-resistant enterobacteriaceae - Wikipedia)
By Jen Christensen and Debra Goldschmidt, CNN
Thu May 26, 2016
'Nightmare' drug-resistant CRE found in U.S. woman - CNN.com
Cases have been found internationally, now here.
Many (if not all) bacterial bugs, it seems, can get resistance on the genetic level.
(see Carbapenem-resistant enterobacteriaceae - Wikipedia)
By Jen Christensen and Debra Goldschmidt, CNN
Thu May 26, 2016
'Nightmare' drug-resistant CRE found in U.S. woman - CNN.com
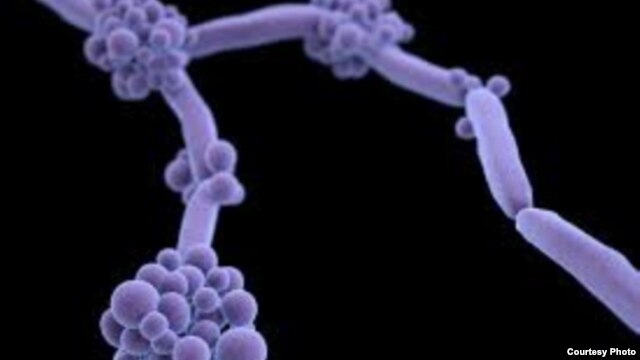
The United States' first known case of a superbug that cannot be killed by any existing antibiotic was announced Thursday by the U.S. Department of Defense. Centers for Disease Control and Prevention Director Dr. Tom Frieden announced the case at the National Press Club in Washington.
A 49-year-old Pennsylvania woman developed a carbapenem-resistant Enterobacteriaceae, or CRE, infection. It's a rare infection but one that Frieden labeled "a nightmare bacteria."
It's resistant to every known antibiotic, even Colistin, which doctors sometimes use as a last resort when other antibiotics fail.
The woman went to a clinic in Pennsylvania, and a sample was forwarded to Walter Reed National Military Medical Center. No other details were available, including how the woman became infected. She has not traveled outside the United States within the past five months.
The bacteria have been identified in other infections outside the United States. Doctors saw a case in the United Kingdom in 2008 and cases in Italy and China.
CRE infections are incredibly difficult to treat and can quickly become deadly. One report suggests that this kind of infection can result in the deaths of half the patients who become infected.
Antibiotic resistance has become a growing problem in this country. The World Health Organization has warned that it is one of the biggest threats to global health today.
Frieden warned that although this is the first CRE case in the United States, we should expect to see more such superbugs in the near future. Frieden, who often warns doctors against overuse of antibiotics, urged scientists to develop new drugs quickly.
Each year in the United States, at least 2 million people become infected with other kinds of bacteria that can't be beat with most antibiotics, and at least 23,000 people die each year as a result of those infections, according to the CDC.
"The medicine cabinet is empty for some patients," Frieden said. "It is the end of the road unless we act urgently."
A 49-year-old Pennsylvania woman developed a carbapenem-resistant Enterobacteriaceae, or CRE, infection. It's a rare infection but one that Frieden labeled "a nightmare bacteria."
It's resistant to every known antibiotic, even Colistin, which doctors sometimes use as a last resort when other antibiotics fail.
The woman went to a clinic in Pennsylvania, and a sample was forwarded to Walter Reed National Military Medical Center. No other details were available, including how the woman became infected. She has not traveled outside the United States within the past five months.
The bacteria have been identified in other infections outside the United States. Doctors saw a case in the United Kingdom in 2008 and cases in Italy and China.
CRE infections are incredibly difficult to treat and can quickly become deadly. One report suggests that this kind of infection can result in the deaths of half the patients who become infected.
Antibiotic resistance has become a growing problem in this country. The World Health Organization has warned that it is one of the biggest threats to global health today.
Frieden warned that although this is the first CRE case in the United States, we should expect to see more such superbugs in the near future. Frieden, who often warns doctors against overuse of antibiotics, urged scientists to develop new drugs quickly.
Each year in the United States, at least 2 million people become infected with other kinds of bacteria that can't be beat with most antibiotics, and at least 23,000 people die each year as a result of those infections, according to the CDC.
"The medicine cabinet is empty for some patients," Frieden said. "It is the end of the road unless we act urgently."