Drug-resistant food poisoning is now in the US - AOL.com
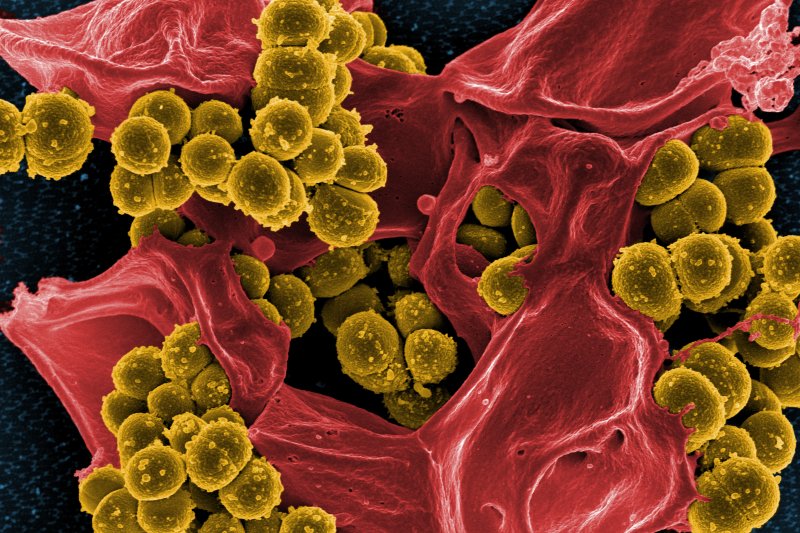
Food poisoning bug making the rounds. Looks like a nasty one cuz it fights off the drug to kill it.
Food poisoning bug making the rounds. Looks like a nasty one cuz it fights off the drug to kill it.