Yes, they are in fact finding savings in Medicare.
What does this mean ?
Savings that were there to be had absent the ACA ?
Savings created by the ACA ?
As I've stressed in this thread several times, we're in the midst of something of a rolling revolution in the organization, delivery, and financing of health care in the U.S. And yes, the ACA is a significant factor in this change and its primary tool for being an agent of change is reforms to the Medicare program.
Payers, led by Medicare, are starting to pay health care providers to do better, be better, and do it while holding down cost growth. The financial incentives are changing, which in turn means the delivery strategies can change with them--toward team-based care, coordination across health care settings, with an eye toward prevention and better management of health conditions.
At a high level, the ACA demands savings. But it isn't just an edict from on high, it also contains a number of tools to make that feasible and accomplish it.
The law created financial incentives to prevent avoidable re-hospitalizations. Lo and behold, historic drops in preventable readmissions followed as hospitals got a lot more interested in preserving the health of their patients post-discharge.
Obamacare Incentives Slow Hospitals' Revolving Door
Then Redd, like more than 600 other Mount Sinai patients over the past three years, was singled out as a high-risk patient and assigned to one of 27 social workers focused on keeping patients out of the hospital. Mount Sinai created the program after the Affordable Care Act set up an incentive system to provide hospitals extra money for keeping people healthy, and penalize them for having too many patients readmitted too soon.
It offered incentives for the creation of new organizations that re-organized care delivery, eliminating some of the discord that drove up health costs:
Medicare Seniors Like ObamaCare's Team Approach
As the U.S. health care system moves away from fee-for-service medicine to more accountable care that uses a team of health professionals, seniors covered by Medicare say they are okay with these new models that include nurses, social workers and other allied health professionals in the front lines of their treatment, according to a new analysis.
Increasingly, the Medicare health insurance program for the elderly as part of the Affordable Care Act is moving to a system that rewards doctors and hospitals for working together to improve care. By contracting with entities known as accountable care organizations and patient-centered medical homes, the providers use a team approach that can involve lower cost providers and allied health professionals to provide seniors with more attention while at the same time keeping them healthy and out of more expensive care settings.
There are hundreds of these organizations now, serving millions of Medicare patients (and others).
Paying Doctors to Shun Hospital
In an attempt to tame growing Medicare costs, the Affordable Care Act encourages doctors and hospitals to form groups called accountable care organizations, or ACOs. The idea is to get doctors, hospitals, nursing homes, and other providers to work together to treat Medicare patients. They’re supposed to avoid unneeded or redundant procedures and emphasize preventive care and chronic-disease management. These alliances typically invest in electronic health records to track patient treatments and hire social workers to make sure patients take their medic
The ACA started tying Medicare payments to the quality of care offered, putting health care providers on the financial hook for the product they sold.
Do Structural Changes Drive the Recent Health Care Spending Slowdown? New Evidence
Value-based purchasing of hospital services has had a significant impact on hospital behavior. Hospitals are highly sensitive to changes in financial incentives. Movement away from a preponderance of fee-for-service payments is also likely to permanently alter hospital behavior. For instance, emphasis on reduced readmissions has reportedly changed how hospital managers think about care delivery, from the care delivered within their four walls towards coordinating care outside their four walls as they track patients as they return to the community or to various post acute care settings.
An observation is that hospitals and other providers are being called to change their care delivery models and business models as payment systems evolve. In a general sense this is leading to a re-engineering of care- slow to start with, but gaining momentum over time. The ACA, with its call for CMMI grants, shows the potential magnitude of private and public sector experiments with alternative organizational forms such as ACOs and medical homes in combination with payment system incentives in the form of payments for value, payment bundling and capitation and prompting the health care industry to reconsider delivery models that reduce incentives for volume of care under fee-for- service. As organizational forms and payment models evolve, augmentation of computing powers and more ready access to “big data” claims files emphasizes an ability to better understand the consequences of change in terms of clinical and economic outcomes.
And they're only stepping up their game from here on:
HHS sets goals for expanding new Medicare payment models
The Obama administration wants 30% of payments for traditional Medicare benefits to be tied to alternative payment models such as accountable care organizations by the end of 2016. The administration also has set a goal of hitting 50% by the end of 2018.
The administration wants even larger portions of hospital payments to be tied to quality- or value-based payment models. HHS indicated that it wants 85% of Medicare's hospital payments made through programs such as the Hospital Value-Based Purchasing Program or the Hospital Readmissions Reduction Program by the end of 2016. That threshold kicks up to 90% two years later.
It is the first time that the federal agency has set specific goals for overhauling the payment system for standard Medicare beneficiaries, which has traditionally relied on a fee-for-service model. That system has long been criticized for providing economic incentives for providers to offer a greater volume of care regardless of outcomes. Currently, 20% of Medicare payments for traditional beneficiaries are made through alternative payments models, which also include bundled payment arrangements, according to HHS.
“We believe these goals can drive transformative change, help us manage and track progress and create accountability for measurable improvement,” HHS Secretary Sylvia Mathews Burwell said in a statement announcing the targets.
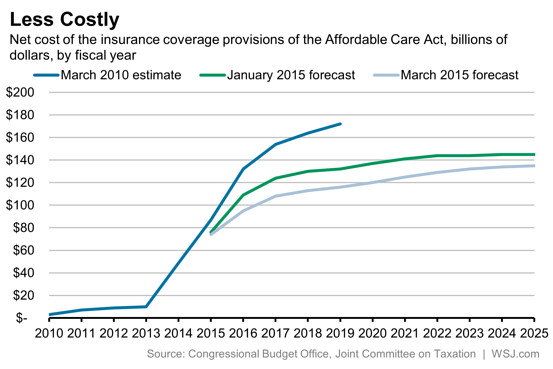
The savings are real, the changes are real. And this stuff didn't exist pre-ACA. It's pretty unlikely that per capita Medicare spending would now be
falling (as it now is) in the absence of the Affordable Care Act.
Are there parts of Obamacare that have yet to be implemented ?
At this point, not really. Some small fraction of the population is still in a grandfathered pre-ACA health plan. A small minority of employees are working for employers who won't be subject to the employer mandate for a few more months. The only large remaining piece is the excise tax on high-cost health plans (due to be implemented in 2018).