This is not just for robotics -- but has large promise in prosthetic devices.. The bigger part here is discovering the signal coding and communications for a touch as seen by the nerve cells and then it becomes possible to transmit that to the brain as a seamless replacement for lost limbs/fingers/toes..
Stanford engineers create artificial skin that can send pressure sensation to brain cell
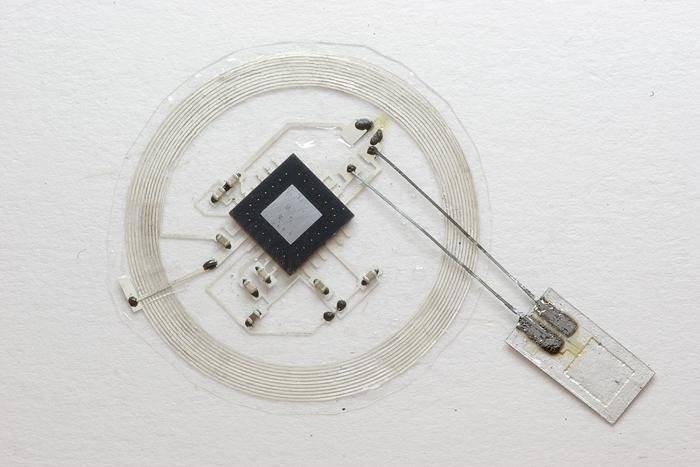
Stanford engineers have created a plastic "skin" that can detect how hard it is being pressed and generate an electric signal to deliver this sensory input directly to a living brain cell.
Shenan Bao, a professor of chemical engineering at Stanford, has spent a decade trying to develop a material that mimics skin's ability to flex and heal, while also serving as the sensor net that sends touch, temperature and pain signals to the brain. Ultimately she wants to create a flexible electronic fabric embedded with sensors that could cover a prosthetic limb and replicate some of skin's sensory functions.
Bao's work, reported today in Science, takes another step toward her goal by replicating one aspect of touch, the sensory mechanism that enables us to distinguish the pressure difference between a limp handshake and a firm grip. See video here.
"This is the first time a flexible, skin-like material has been able to detect pressure and also transmit a signal to a component of the nervous system," said Bao, who led the 17-person research team responsible for the achievement.
Benjamin Tee, a recent doctoral graduate in electrical engineering; Alex Chortos, a doctoral candidate in materials science and engineering; and Andre Berndt, a postdoctoral scholar in bioengineering, were the lead authors on the Science paper.
Stanford engineers create artificial skin that can send pressure sensation to brain cell
Stanford engineers have created a plastic "skin" that can detect how hard it is being pressed and generate an electric signal to deliver this sensory input directly to a living brain cell.
Shenan Bao, a professor of chemical engineering at Stanford, has spent a decade trying to develop a material that mimics skin's ability to flex and heal, while also serving as the sensor net that sends touch, temperature and pain signals to the brain. Ultimately she wants to create a flexible electronic fabric embedded with sensors that could cover a prosthetic limb and replicate some of skin's sensory functions.
Bao's work, reported today in Science, takes another step toward her goal by replicating one aspect of touch, the sensory mechanism that enables us to distinguish the pressure difference between a limp handshake and a firm grip. See video here.
"This is the first time a flexible, skin-like material has been able to detect pressure and also transmit a signal to a component of the nervous system," said Bao, who led the 17-person research team responsible for the achievement.
Benjamin Tee, a recent doctoral graduate in electrical engineering; Alex Chortos, a doctoral candidate in materials science and engineering; and Andre Berndt, a postdoctoral scholar in bioengineering, were the lead authors on the Science paper.