BDBoop
Platinum Member
- Banned
- #1
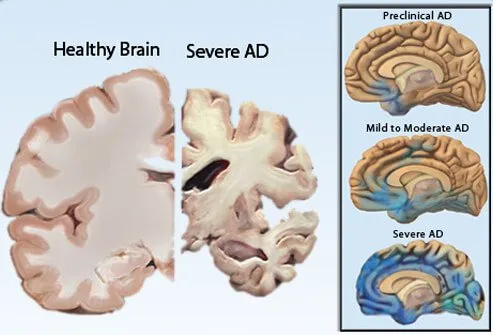
I found this site Alzheimer's Disease and Dementia | Alzheimer's Association because a customer is dealing with her mother's disease. If anybody else is caring for a loved one with dementia, they seem to have a very active community to touch base with, and lots of resources.