USAMomma
Member
- Jul 14, 2010
- 287
- 52
- 16
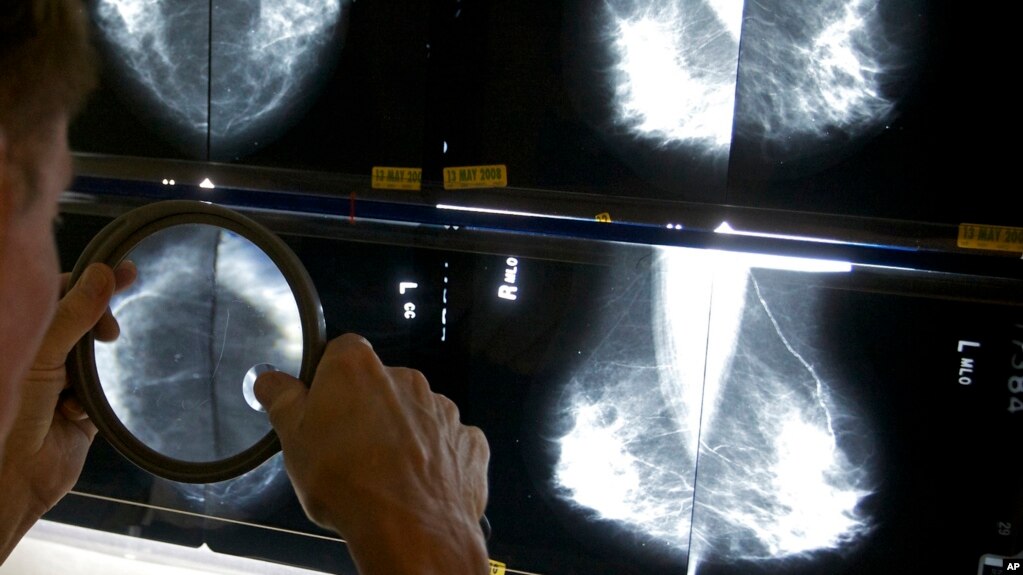
So many rumors and controversies surround breast cancerwhat really causes it, what really prevents itthat it can be hard to know whom to believe.
12 Myths to Ignore About Breast Cancer: Breast cancer myths, debunked - 1 - MSN Health & Fitness - Breast Cancer Slide Show
12 Myths to Ignore About Breast Cancer: Breast cancer myths, debunked - 1 - MSN Health & Fitness - Breast Cancer Slide Show