ScienceRocks
Democrat all the way!
- Banned
- #1
Mutant Superbug Has Been Discovered In The U.S.
The infection resists the treatment of last resort, meaning “the medicine cabinet is empty for some patients,” the CDC director said.
Mutant Superbug Has Been Discovered In The U.S.
05/27/2016 12:36 am ET
If we were a nation that cared about the health of our people we'd spend money on developing the means to beat such a bug. Of course, building schools for little middle eastern kids and handing over military trucks, tanks and other shit is more important.
The infection resists the treatment of last resort, meaning “the medicine cabinet is empty for some patients,” the CDC director said.
Mutant Superbug Has Been Discovered In The U.S.
05/27/2016 12:36 am ET
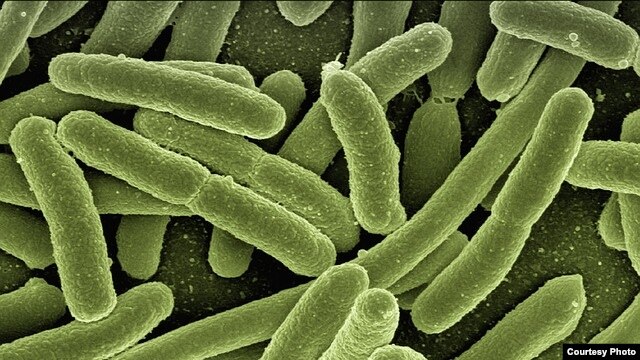
A mutant strain of E. coli, resistant to even the toughest antibiotics, has been found in the United States, federal health officials said Thursday.
The bacteria, discovered last month in a 49-year-old Pennsylvania woman with a urinary tract infection, contains a gene known as mcr-1, making it resistant even to colistin, a decades-old antibiotic that has increasingly been used as a treatment of last resort against dangerous superbugs.
If we were a nation that cared about the health of our people we'd spend money on developing the means to beat such a bug. Of course, building schools for little middle eastern kids and handing over military trucks, tanks and other shit is more important.