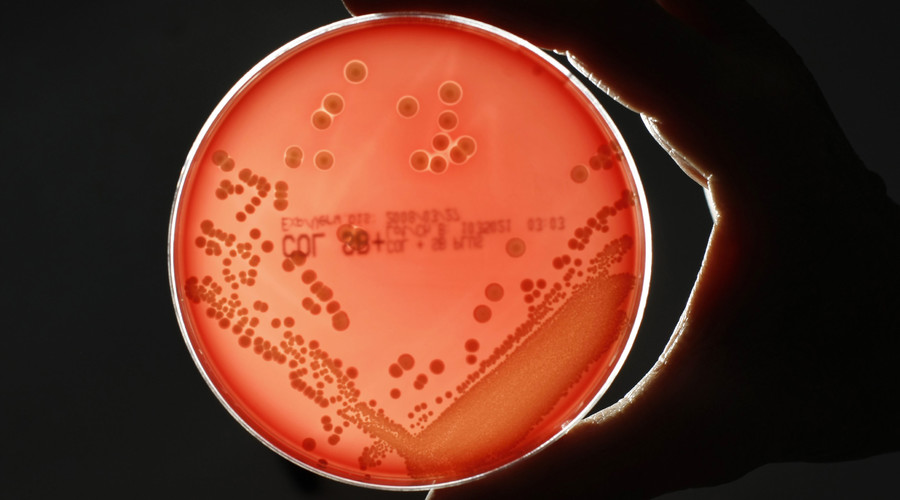
New superbugs are becoming resistant to modern medicines so English scientists went back to a thousand year old manuscript to recreate a cure for eye infection which works against modern strains.
Wonder just how many so-called “Witches Brew” remedies will be found to be effective? Read more @ 1 000-Year-Old Saxon Remedy Kills Superbugs Power Line
Wonder just how many so-called “Witches Brew” remedies will be found to be effective? Read more @ 1 000-Year-Old Saxon Remedy Kills Superbugs Power Line