Arianrhod
Gold Member
- Jul 24, 2015
- 11,060
- 1,076
- 255
Posted in its entirety because the site is membership only:
www.medscape.com
Hospital Readmission Rates Drop Nationally
Ken Terry
September 15, 2016
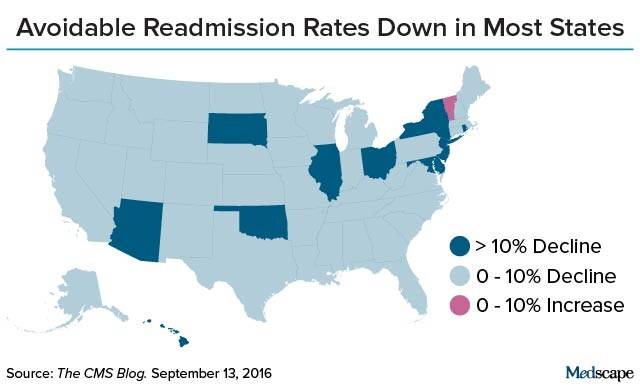
Hospital readmission rates dropped by an average of 8% nationally from 2010 to 2015, the Centers for Medicare & Medicaid Services (CMS) announced on Tuesday. The number of avoidable 30-day readmissions of Medicare patients dropped in 49 states and the District of Columbia, according to CMS. In 43 states, the readmission rates fell by more than 5%, and in 11 states, by more than 10%.
Writing in the CMS blog, Patrick Conway, MD, principal deputy administrator and chief medical office of CMS, and Tim Gronniger, deputy chief of staff of CMS, attributed the drop in the readmission rate primarily to the Hospital Readmissions Reduction Program. Enacted as part of the Affordable Care Act (ACA) in 2010, the program reduces Medicare reimbursement rates for hospitals with higher than expected 30-day readmission rates for targeted clinical conditions, such as acute myocardial infarction (AMI), heart failure, and pneumonia.
Secondarily, the CMS officials said, agency quality improvement initiatives, such as the Partnership for Patients, have made a difference in the readmission rate. The Partnership aims to make hospital care safer and improve the quality of care for individuals as they move from one healthcare setting to another.
CMS estimated that Medicare beneficiaries avoided 100,000 readmissions in 2015 alone compared with what they would have been if readmission rates had remained at 2010 levels. Since 2010, Medicare beneficiaries have avoided about 565,000 readmissions, according to the Department of Health and Human Services.
Among states, the largest declines in readmission rates were seen in New Jersey, which saw a 13.3% drop; Hawaii, 13.4%; and Illinois, 12.1%. In contrast, Vermont was the only state with an increase in readmissions, but the change was modest at just 0.7%.
Despite the overall percentage decline, the absolute national readmission rate did not fall substantially. According to a chart that CMS provided, it dropped only from a little over 19% to a bit under 18% from 2010 to 2015.
In a New England Journal of Medicine study, published earlier this year, that examined the changes in readmission rates between 2007 and 2015 for AMI, heart failure, and pneumonia — three of the targeted conditions — CMS researchers found that risk-adjusted rates of readmissions for the targeted conditions dropped from 21.5% to 17.8%, and rates for nontargeted conditions declined from 15.3% to 13.1%.
The readmission rates for targeted conditions were already declining slightly before the passage of the ACA but dropped more significantly from 2010 to 2012, according to the authors, led by Rachael B. Zuckerman from the Office of the Assistant Secretary for Planning and Evaluation, Department of Health and Human Services, Washington, DC. After that, they continued to fall, but at a slower rate.
"Presumably, hospitals made substantial changes during the study period but could not sustain such a high rate of reductions in the long term," the authors surmised.
Some critics of CMS' Hospital Readmission Reduction Program have speculated that the readmission rates have not dropped as much as reported because some Medicare patients came back to the hospital for observation stays. Hospitals were doing this, some experts suggest, to avoid incurring readmission penalties.
But Zuckerman and colleagues found that rates of observation stays increased for both targeted and nontargeted conditions from 2007 to 2015. No significant increases in observation stays for targeted conditions were observed after the ACA's passage. The researchers concluded that there was no significant correlation between the change in readmission rates and the change in observation-service use.
The Hospital Readmission Reduction Program has penalized hospitals with higher-than-expected 30-day readmission rates for AMI, heart failure, and pneumonia since October 2012, the start of fiscal year (FY) 2013. Total knee or hip replacement and chronic obstructive pulmonary disease became targeted conditions starting in FY 2015.
The calculation of hospital penalties is based on the readmission performance for the previous 3 years, which explains why hospitals tried hard to reduce readmission rates beginning in 2010. The initial penalty in FY 2013 was 1% of a hospital's diagnosis-related-group payments. Since FY 2015, the penalty has increased to 3%.
For more news, join us on Facebook and Twitter
Medscape Medical News © 2016 WebMD, LLC
Send comments and news tips to [email protected].
Cite this article: Hospital Readmission Rates Drop Nationally. Medscape. Sep 15, 2016.
While the "opposition" bases its "knowledge" on YouTube sound bites and "$8,500!!!!11!" the Real World presents those inconvenient things called facts.
There's even a pretty little map to go with the article:
Thanks, Obama.
www.medscape.com
Hospital Readmission Rates Drop Nationally
Ken Terry
September 15, 2016
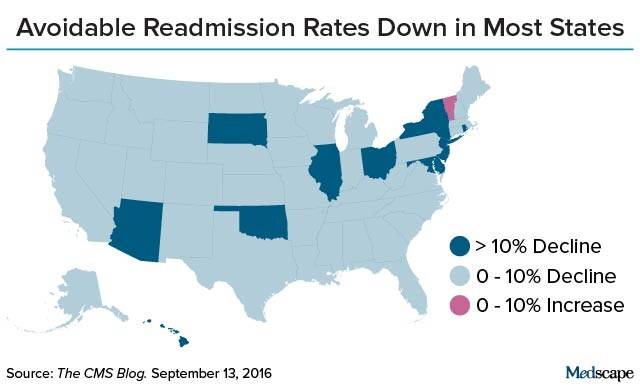
Hospital readmission rates dropped by an average of 8% nationally from 2010 to 2015, the Centers for Medicare & Medicaid Services (CMS) announced on Tuesday. The number of avoidable 30-day readmissions of Medicare patients dropped in 49 states and the District of Columbia, according to CMS. In 43 states, the readmission rates fell by more than 5%, and in 11 states, by more than 10%.
Writing in the CMS blog, Patrick Conway, MD, principal deputy administrator and chief medical office of CMS, and Tim Gronniger, deputy chief of staff of CMS, attributed the drop in the readmission rate primarily to the Hospital Readmissions Reduction Program. Enacted as part of the Affordable Care Act (ACA) in 2010, the program reduces Medicare reimbursement rates for hospitals with higher than expected 30-day readmission rates for targeted clinical conditions, such as acute myocardial infarction (AMI), heart failure, and pneumonia.
Secondarily, the CMS officials said, agency quality improvement initiatives, such as the Partnership for Patients, have made a difference in the readmission rate. The Partnership aims to make hospital care safer and improve the quality of care for individuals as they move from one healthcare setting to another.
CMS estimated that Medicare beneficiaries avoided 100,000 readmissions in 2015 alone compared with what they would have been if readmission rates had remained at 2010 levels. Since 2010, Medicare beneficiaries have avoided about 565,000 readmissions, according to the Department of Health and Human Services.
Among states, the largest declines in readmission rates were seen in New Jersey, which saw a 13.3% drop; Hawaii, 13.4%; and Illinois, 12.1%. In contrast, Vermont was the only state with an increase in readmissions, but the change was modest at just 0.7%.
Despite the overall percentage decline, the absolute national readmission rate did not fall substantially. According to a chart that CMS provided, it dropped only from a little over 19% to a bit under 18% from 2010 to 2015.
In a New England Journal of Medicine study, published earlier this year, that examined the changes in readmission rates between 2007 and 2015 for AMI, heart failure, and pneumonia — three of the targeted conditions — CMS researchers found that risk-adjusted rates of readmissions for the targeted conditions dropped from 21.5% to 17.8%, and rates for nontargeted conditions declined from 15.3% to 13.1%.
The readmission rates for targeted conditions were already declining slightly before the passage of the ACA but dropped more significantly from 2010 to 2012, according to the authors, led by Rachael B. Zuckerman from the Office of the Assistant Secretary for Planning and Evaluation, Department of Health and Human Services, Washington, DC. After that, they continued to fall, but at a slower rate.
"Presumably, hospitals made substantial changes during the study period but could not sustain such a high rate of reductions in the long term," the authors surmised.
Some critics of CMS' Hospital Readmission Reduction Program have speculated that the readmission rates have not dropped as much as reported because some Medicare patients came back to the hospital for observation stays. Hospitals were doing this, some experts suggest, to avoid incurring readmission penalties.
But Zuckerman and colleagues found that rates of observation stays increased for both targeted and nontargeted conditions from 2007 to 2015. No significant increases in observation stays for targeted conditions were observed after the ACA's passage. The researchers concluded that there was no significant correlation between the change in readmission rates and the change in observation-service use.
The Hospital Readmission Reduction Program has penalized hospitals with higher-than-expected 30-day readmission rates for AMI, heart failure, and pneumonia since October 2012, the start of fiscal year (FY) 2013. Total knee or hip replacement and chronic obstructive pulmonary disease became targeted conditions starting in FY 2015.
The calculation of hospital penalties is based on the readmission performance for the previous 3 years, which explains why hospitals tried hard to reduce readmission rates beginning in 2010. The initial penalty in FY 2013 was 1% of a hospital's diagnosis-related-group payments. Since FY 2015, the penalty has increased to 3%.
For more news, join us on Facebook and Twitter
Medscape Medical News © 2016 WebMD, LLC
Send comments and news tips to [email protected].
Cite this article: Hospital Readmission Rates Drop Nationally. Medscape. Sep 15, 2016.
While the "opposition" bases its "knowledge" on YouTube sound bites and "$8,500!!!!11!" the Real World presents those inconvenient things called facts.
There's even a pretty little map to go with the article:
Thanks, Obama.
