Who wants to eat monkey worms? Yuch!...

Parasitic worms 'treat diarrhoea'
15 November 2012 - Chronic diarrhoea could be treated using parasitic worms, a study of monkeys has suggested.

Parasitic worms 'treat diarrhoea'
15 November 2012 - Chronic diarrhoea could be treated using parasitic worms, a study of monkeys has suggested.
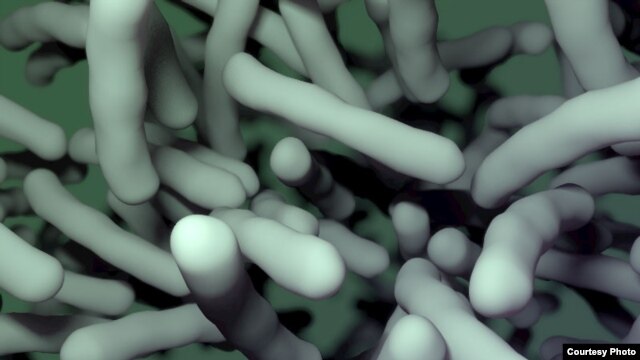
Research published in PLOS Pathogens, suggests the treatment restores gut bacteria to a healthy state. Other work in mice has already suggested conditions such as ulcerative colitis could be treated in this way. A UK expert said parasitic worms were being investigated for a range of conditions, including multiple sclerosis and allergies.
Captivity
Inflammatory bowel diseases, like colitis, are often fuelled by a wrongly targeted response by the immune system to gut bacteria. Such diseases are more common in developed countries - and scientists suggest this is because people in developing countries have more exposure to parasitic worm (helminth) infections and therefore have a natural protection that has evolved as people and worms learnt to co-exist.

Macaque monkeys suffer from a similar bowel condition to humans
Recent studies have used parasitic worms to successfully treat inflammatory bowel disease in humans, but it is unclear exactly how they do this. This latest study looked at monkeys because young macaques kept in captivity often develop chronic diarrhoea that can be hard to treat. Five macaques with diarrhoea were treated with parasitic worms called whipworms.
Tissue samples were taken before and after treatment and it was found the balance of gut bacteria was restored to required levels. And four out of five animals had less diarrhoea and started to gain weight. Dr P'ng Loke, of the New York University Langone Medical Center, who led the study, said: "The idea for treating colitis with worms is not new, but how this therapy might work remains unclear.
More BBC News - Parasitic worms 'treat diarrhoea'