ScienceRocks
Democrat all the way!
- Banned
- #1
New antibiotic cures disease by disarming pathogens, not killing them
October 2, 2012
Read more at: New antibiotic cures disease by disarming pathogens, not killing them
October 2, 2012
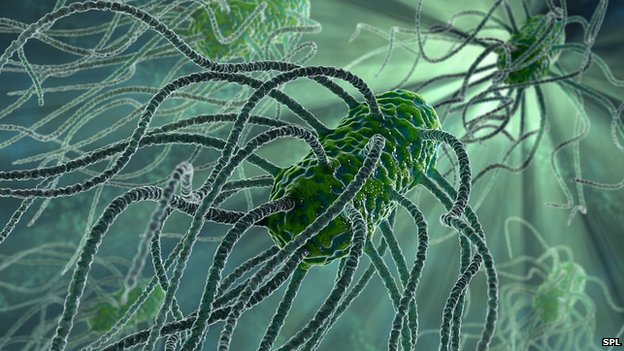
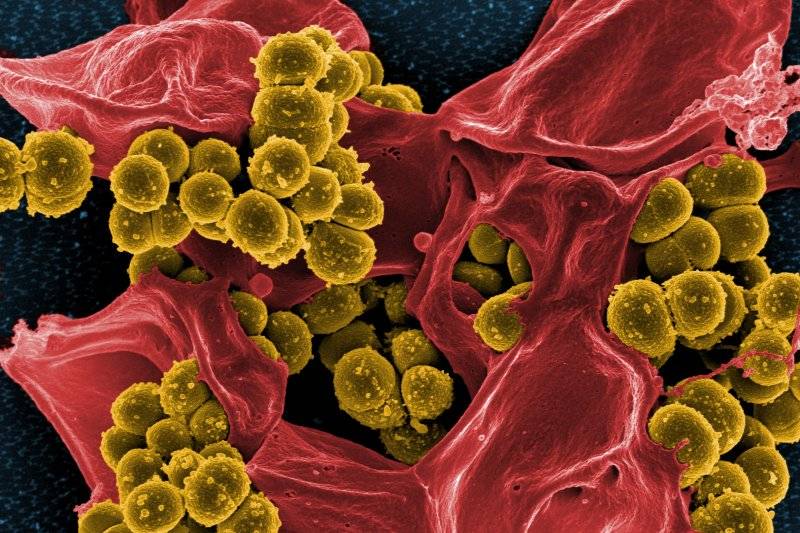
A new type of antibiotic can effectively treat an antibiotic-resistant infection by disarming instead of killing the bacteria that cause it. Researchers report their findings in the October 2 issue of mBio, the online open-access journal of the American Society for Microbiology.
"Traditionally, people have tried to find antibiotics that rapidly kill bacteria. But we found a new class of antibiotics which has no ability to kill Acinetobacter that can still protect, not by killing the bug, but by completely preventing it from turning on host inflammation," says Brad Spellberg of the UCLA Medical Center and David Geffen School of Medicine, a researcher on the study. New drugs are badly needed for treating infections with the bacterium Acinetobacter baumannii, a pathogen that most often strikes hospital patients and immune- compromised individuals through open wounds, breathing tubes, or catheters.
The bacterium can cause potentially lethal bloodstream infections. Strains of A. baumannii have acquired resistance to a wide range of antibiotics, and some are resistant to every FDA-approved antibiotic, making them untreatable. Spelling and his colleagues found that in laboratory mice it was possible to mitigate the potentially lethal effects of the bacterium by blocking one of its toxic products rather than killing it. "We found that strains that caused the rapidly lethal infections shed lipopolysaccharide [also called LPS or endotoxin] while growing. The more endotoxin shed, the more virulent the strain was," says Spellberg. This pinpointed a new therapy target for the researchers: the endotoxin these bacteria shed in the body.
Read more at: New antibiotic cures disease by disarming pathogens, not killing them