TruthOut10
Active Member
- Dec 3, 2012
- 627
- 100
- 28
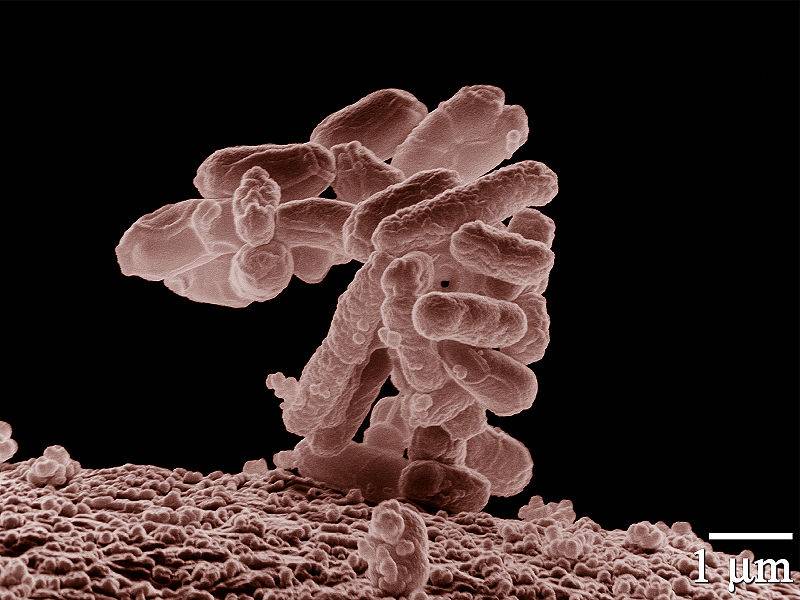
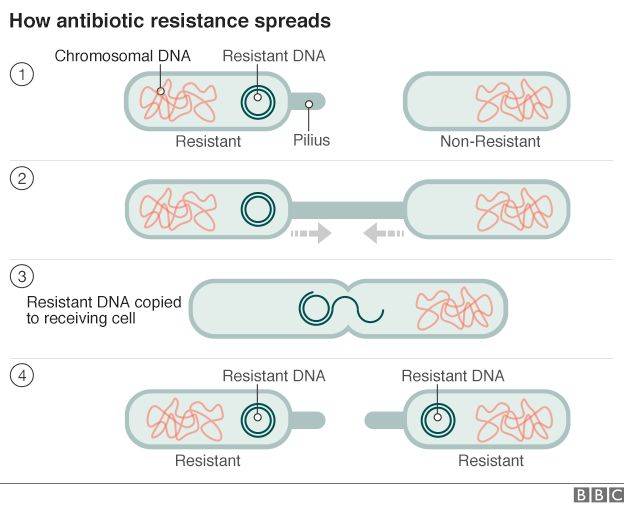
The fears of major health organizations have come true: Gonorrhea that is immune to the last remaining effective oral antibiotic has been detected in at least nine North American patients, meaning the era of "incurable" gonorrhea could be close.
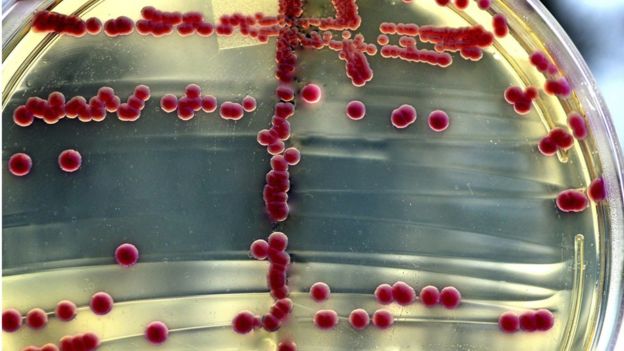
In a study released Tuesday in the Journal of the American Medical Association, a group of scientists led by Vanessa Allen of Public Health Ontario, found that 6.7 percent of patients with gonorrhea at a Toronto clinic still had the disease after a round of cephalosporins, the last effective oral antibiotic used to treat the disease. Of 133 patients who returned for a "test of cure" visit, nine remained gonorrhea-positive. This is the first time cephalosporin-resistant gonorrhea has been found in humans in North America.
[RELATED: How to Teach Your Kids About Sex]
Last year, both the World Health Organization and the Centers for Disease Control warned that untreatable gonorrheathe world's second most common sexually transmitted infectioncould soon be a reality as the bacteria showed increasing resistance to cephalosporins in lab tests.
"These are the clinical cases we've been waiting for," Allen says. "This is the translation of the lab information into what the clinical consequence is."
Previously, there had been a couple individual case reports of untreatable gonorrhea cases in the United Kingdom, Austria, France, Norway, and Japan. In an accompanying editorial, Robert Kirkcaldy of the CDC writes that gonorrhea is quickly becoming a more threatening disease.
[FLASHBACK: CDC Warns Untreatable Gonorrhea Coming]
"Cephalosporin treatment failures have now been documented in North America," he writes. "Although this milestone was expected, its arrival is deeply troubling."
Gonorrhea is estimated to infect close to 700,000 Americans each year. Symptoms include painful urination, abdominal pain, genital discharge, itching, and infertility in women. Women who have both HIV and gonorrhea are more likely to pass HIV to their offspring than women with just HIV.
First Antibiotic-Resistant Gonorrhea Cases Detected in North America - US News and World Report
In a study released Tuesday in the Journal of the American Medical Association, a group of scientists led by Vanessa Allen of Public Health Ontario, found that 6.7 percent of patients with gonorrhea at a Toronto clinic still had the disease after a round of cephalosporins, the last effective oral antibiotic used to treat the disease. Of 133 patients who returned for a "test of cure" visit, nine remained gonorrhea-positive. This is the first time cephalosporin-resistant gonorrhea has been found in humans in North America.
[RELATED: How to Teach Your Kids About Sex]
Last year, both the World Health Organization and the Centers for Disease Control warned that untreatable gonorrheathe world's second most common sexually transmitted infectioncould soon be a reality as the bacteria showed increasing resistance to cephalosporins in lab tests.
"These are the clinical cases we've been waiting for," Allen says. "This is the translation of the lab information into what the clinical consequence is."
Previously, there had been a couple individual case reports of untreatable gonorrhea cases in the United Kingdom, Austria, France, Norway, and Japan. In an accompanying editorial, Robert Kirkcaldy of the CDC writes that gonorrhea is quickly becoming a more threatening disease.
[FLASHBACK: CDC Warns Untreatable Gonorrhea Coming]
"Cephalosporin treatment failures have now been documented in North America," he writes. "Although this milestone was expected, its arrival is deeply troubling."
Gonorrhea is estimated to infect close to 700,000 Americans each year. Symptoms include painful urination, abdominal pain, genital discharge, itching, and infertility in women. Women who have both HIV and gonorrhea are more likely to pass HIV to their offspring than women with just HIV.
First Antibiotic-Resistant Gonorrhea Cases Detected in North America - US News and World Report